Whether screen general public or not
Introduction of Taiwan’s precautionary measures
Due to the outbreak of COVID-19, millions of people have lived in fear of being infected by this contagious and fatal virus. Almost every country in the world has taken as many preventive measures as possible to reduce the chance of infection, include staying at home, avoiding crowded places, keeping social distance and washing hands, etc. It is undoubtedly that making those multiplicative preventive efforts may lead to more avoided new cases down the line, which in turn can stop the outbreak in its tracks.

Taiwan, probably the most successful country in battling with coronavirus, have similar sized populations of about 24 million people as Australia and even much closer to China than any country else. Ten weeks on from January 25, Australia has almost 5,000 confirmed cases, while Taiwan has less than 400. This is because Taiwan’s CDC has been on high alert to a mysterious pneumonia outbreak in Wuhan since the end of 2019 when other parts of the world have not. The Taiwanese government also made several aggressive decisions such as blocking exports of surgical masks to conserve supplies, banning travel to many parts of China, and even quarantining people who have specific travel history which later proved wise.
Debate on whether screening general public or not
However, there was a fierce debate in Taiwan recently on whether screening general public for COVID-19 or not. Although Taiwan has already no new confirmed cases in four continuous days, the majority of people still worry about the asymptomatic cases that conceal themselves in the community. While some people argue that screening general public for COVID-19 is ineffective and wasteful precautionary measures to further decrease healthcare capacity, other people still suggest that the Ministry of Health and Welfare (MOHW) should screen 24 million people case by case to identify the hidden COVID-19 carriers. Thus, as a student majoring public health, I am going to describe why we DO NOT need to screen all of people.
The reason why we DO NOT NEED to screen all of people
Before we decide whether take this measure or not, we have to know what testing technique do we use now. The following table summarize the examining methods we use nowadays to detect COVID-19.
| Testing method | testing time | Timing | Sensitivity | Specificity |
|---|---|---|---|---|
| RT PCR | 2 to 4 days | Early onset | > 95 % | > 95 % |
| Fast screening (Antigens) | 15 mins | Early onset | 70 % | > 95 % |
| Fast screening (Antibody) | 15 mins | 7 days after onset | 75 % | > 95 % |
Time & Money
Based on the data from the National Health Command Center (NHCC), RT-PCR is approximately 100 U.S. dollars per person. Imagine if we screen 24 million people case by case by using RT-PCR, it totally costs around 2.3 billion U.S. dollars. That is definitely not a small amount of money and the huge numbers of specimens will be a heavy burden to Medical Laboratory Technician. Moreover, if we use fast screening rather than RT-PCR, we may save a lot of money to 4600 million U.S. dollars. However, the test results will be inaccurate because lower sensitivity would increase the numbers of false negative and false positive.
Inaccurate Results
In medical testing, and more generally in binary classification, a false positive and false negative are errors commonly in data reporting in which a test result improperly indicates the presence of a condition. Furthermore, the numbers of those errors will affect by the sensitivity and specificity of the testing tool and the prevalence rate of the illness.
-
Sensitivity (also called true positive rate): measures the proportion of actual positives that are correctly identified as such.
-
Specificity (also called true negative rate): measures the proportion of actual negatives that are correctly identified as such.
-
Prevalence: the number of disease cases present in a particular population at a given time.
If we would like to believe the positive testing result actually means the patient was infected, we may need to understand the Positive Predictive Value (PPV). If Positive Predictive Value is 50%, it means that when we see two positive testing result, one person must be misdiagnosed. The formula of positive predictive value is below.

Thus, imagining that we have a strong testing tool with 95% Sensitivity and 95% Specificity, the prevalence rate of COVID-19 is still less than 3% in Taiwan which makes the PPV of Taiwan equals to 37%. 37% of PPV is definitely not a good index for diagnose the hidden carriers but only increase the anxiety of the general public. However, if we select risk population by using disease reporting system. The target audience will be narrow down and the prevalence rate may rise to around 30% and therefore the PPV will also rise to 90% which is a nearly perfect index we can believe in.
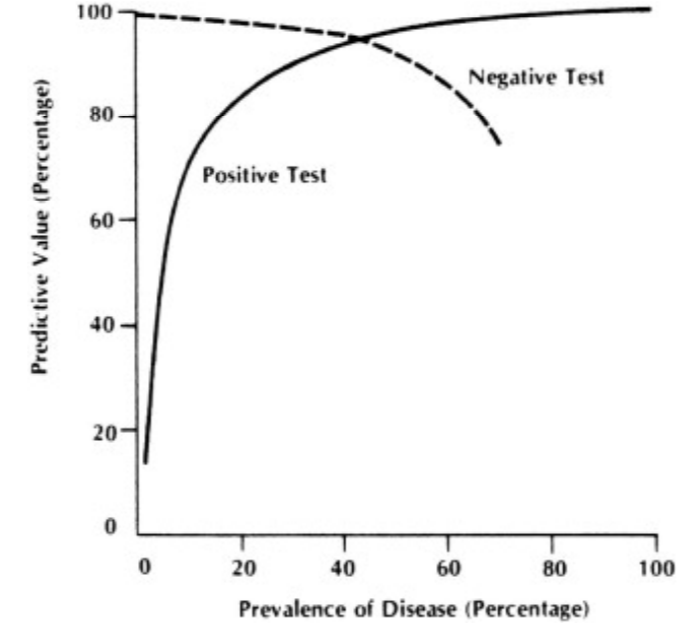
Relationship between disease prevalence and predictive value in a test with 95% sensitivity and 85% specificity. (From Mausner JS, Kramer S: Mausner and Bahn Epidemiology: An Introductory Text. Philadelphia, WB Saunders, 1985, p. 221.)
Reference
- Taiwan’s battle against coronavirus began in late 2019
- Taiwan’s coronavirus response is among the best globally
- Sensitivity and Specificity
- Prevalence
- 武漢肺炎》阿中開課了!
- Taiwan Public Television Service
- PennState University Epidemiological Research Methods
- Measurement Brings Meaning to Population Health(AHIMA)
